“I’m full of
energy—and
unstoppable!”
Diabetes

Springboard to your healthiest self yet!

You have what it takes to rein in your diabetes and achieve your goal numbers. Start by partnering with your care team to create the treatment plan that yields results!
Receiving a diagnosis of type 2 diabetes can feel overwhelming, but it can also be the beginning of a journey toward better health. By making small, positive changes every day, you have the power to take control of your future.
What’s more, today we understand diabetes—and how to manage it—better than ever.
Just ask Nancy Wernick Topiol, who had revamped her diet and started exercising when diagnosed with diabetes a decade ago, but still couldn’t bring her A1C (an average measure of blood sugar levels from the past three months) back down to where it should be. Now, with the help of a GLP-1 RA medication, Nancy is thrilled that her A1C level has dropped to the lowest it’s ever been.
__
Take a stand today!
No matter where you are in your diabetes journey, it’s not too late to get inspired by Nancy as well as Brian and Roger, who share their own blood sugar-lowering strategies here. And in this guide, you’ll find even more tools and tips that can help you along the way. But first, let’s take a closer look at diabetes, what it is and how it affects your body.
__
What is diabetes?
Diabetes is a metabolic disorder that disrupts your body’s ability to produce or use insulin, which causes blood sugar levels to rise. Normally, beta cells, found in the pancreas, make insulin—the hormone that helps blood sugar enter cells to be used for energy. (Hormones are a natural chemical found in the body.)
In type 1 diabetes, beta cells are destroyed by the immune system, so the body does not make enough insulin. In type 2 diabetes, beta cells either don’t produce enough insulin and/or the body’s cells do not respond correctly to insulin (known as insulin resistance).
When blood sugar is unable to enter the body’s cells, it builds up in the bloodstream. Over time, excess blood sugar can lead to body-wide damage, including vision loss, heart disease, kidney disease and nerve damage.
Early symptoms of diabetes can include:
- frequent urination
- slow-healing wounds
- blurry vision
- fatigue
- increased thirst and hunger
- weight loss
- tingling in hands and/or feet
- very dry skin
- increased infections
__
Medicine can help
If you have type 1 diabetes, you will need to use insulin to treat the condition. If you have type 2 diabetes, oral medications, non-insulin injectables and/or insulin can help you manage your blood sugar levels. (Click here for information on medication options for people with type 2 diabetes.)
__
What that means
Work with your diabetes care team to identify your blood sugar and A1C goals, and create an action plan to achieve them. Lifestyle changes are also important, so be sure to discuss those topics with your provider, as well.
A special concern for people of color
37 million American have diabetes—and that number is on the rise, especially in Black, Hispanic, Native American and Asian Communities.
The rate of diabetes in Black people is 60% higher compared with White people, more than 50% higher in Hispanics and Native Americans and more than 40% higher in Asian Americans.
What does that mean for you? If you are a person of color and have experienced any symptoms, be sure to tell your healthcare provider and ask that your blood sugar levels be tested.
Luckily, getting prompt and effective treatment can help stave off complications for all people with diabetes.
How medicines can help
The good news for people with type 2 diabetes? Today’s treatments can help you thrive! Ask your diabetes care team if these options are right for you.
Diabetes pills
Metformin decreases blood sugar made by the liver.
Oral glucagon-like peptide receptor agonists (GLP-1 RAs) increase insulin secretion, slow stomach emptying, and lead to reduced food intake and feeling full, with low risk of hypoglycemia (low blood sugar). An injectable form is also available.
Sodium-glucose co-transporter 2 (SGLT2) inhibitors promote the release of excess blood sugar through urine.
Dipeptidyl peptidase-4 (DPP-4) inhibitors prevent breakdown of a blood-sugar lowering compound.
Thiazolidinediones (TZDs) increase how your body responds to insulin.
Non-insulin Injectable Medicines
Injectable GLP-1 RAs increase insulin secretion, slow stomach emptying, and lead to reduced food intake and feeling full, with low risk of hypoglycemia. An oral form is also available.
Glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA combinations include GIP, a hormone that stimulates insulin secretion in response to food, as well as a GLP-1 RA to help your body better manage your blood sugar levels.
Insulin Injections
Insulin helps your body take up blood sugar into cells and helps the liver to store sugar.
Basal, or long-acting, insulin is typically taken once a day and acts slowly over 24 hours.
Bolus, or rapid-acting, insulin is taken before meals to prevent blood sugar increases after eating.
Combination Injectable Medicines
Insulin and GLP-1 RAs can be combined in a fixed-dose pen. The insulin helps keep blood sugar levels within target range, while the GLP-1 RA helps the pancreas release insulin after eating.
Trouble remembering your meds or appointments? Use the calendar on your phone or tablet to keep track of daily meds, healthcare appointments and tests. Even better, synchronize your calendar with your loved ones to keep you both up-to-date.

“Now we’re in control of our diabetes journey!”

After decades of struggling with their health, Nancy, Brian and Roger paved their own paths to wellness. Now, thanks to medications and lifestyle tweaks, they’re feeling better than ever. Here, they share the tricks that made all the difference. —by Diane Herbst
“I’m full of energy—and unstoppable!”
____________________
NANCY WERNICK TOPIOL, 64
JACKSON, NJ
Most days, Nancy Wernick Topiol can be found walking four miles with a friend through her community in Jackson, NJ, or taking high-intensity interval training classes. At home, the retired teacher likes to cook up tasty whole-food, high-protein meals that are low in sugar. And when she’s not busy with that, Nancy travels to Florida to visit her 32-year-old daughter, Marla, and the pair take hours-long brisk walks. “I feel really good,” says the 64-year-old, “so full of energy!”
It’s a far cry from a decade ago, when Nancy ate an abundance of processed foods. She would huff and puff when she walked even small distances as she carried 270 pounds on her 5-foot frame. And a routine blood test showed her lifestyle was taking a toll: Her A1C—which measures a person’s average blood sugar levels over the previous three months—was 8.7%. (A normal A1C level is below 5.7% , 5.7% to 6.4% indicates pre-diabetes and 6.5% and above indicates diabetes.) Nancy was officially diagnosed with type 2 diabetes.
“I felt exhausted all the time,” says Nancy, who at the same time was diagnosed with sleep apnea. “I felt like I was walking around with an anvil on my head.”
“I was nervous to make changes”
Nancy was no stranger to diabetes—her mother, father and many of her paternal relatives had had the condition as well. “I always knew in the back of my head it was in the cards,” she says. “But in the past, any attempt to ‘get healthy’ had meant going on an extremely restrictive diet, which I’d eventually give up on and gain all the weight back.”
This time, though, things were different. Her endocrinologist prescribed a medication to help lower her blood sugar and sent her to a nutritionist, who gave Nancy a list of healthy foods to eat. “It was good in that the list focused on what I could eat, and from then,” she says, “something just sort of clicked.”
“I learned what worked for me”
Determined not to repeat the mistakes of her past, Nancy began making slow changes instead of resorting to extreme dieting.
“I started investigating healthy food choices, swapping out foods high in carbs for vegetables and high-protein pasta and working on portion control, because whatever you put in front of me, I would eat.” At restaurants, Nancy immediately asked for a takeout doggy bag and cut her portion in half, only eating the food remaining on her plate. She learned that taking a bite of food and then following it with a sip of water helped her feel full.
And instead of making drastic cuts, she made small ones—things like just eliminating sugary sodas to start. “I thought, 'You know what, Nancy, you have to make a lifestyle change,' ” she recalls. “ ‘Diets’ don’t work. If you go on a ‘diet,’ you feel like you’re depriving yourself. By doing small changes and swaps, I never felt deprived.”
Nancy also joined a gym and started lifting weights under the guidance of a trainer. These small, consistent changes added up—Nancy’s A1C went down to 6.4%, and she dropped 90 pounds.
“Now I’m in charge of my health!”
But then in 2022, her weight loss plateaued, and her A1C rose to 7.3%. At the same time, Nancy read about GLP-1 receptor agonists (GLP-1 RAs), and how they could help with lowering blood sugar levels. Seeing that Nancy met the appropriate requirements, her healthcare provider added the medication to her regimen.
The new medication helped lower her A1C to 5.9%, “the lowest it’s ever been,” she says. And her sleep apnea disappeared.
Now, thanks to her lifestyle changes and new treatment plan, she’s lost a total of 120 pounds and has her diabetes under control—and she loves sharing her story with others. “Everybody is so proud of me because it was a struggle,” she says. “I lost a whole person! Life is a journey, and this is part of that journey. People are so hard on themselves, and I learned that if I make a mistake, so be it—it doesn’t define me, and I get back on track and do better.”
Small steps that make a BIG difference
Nancy’s goal was to get her diabetes and weight under control. “I realized that if I make small changes, it becomes a part of life and I don’t feel deprived,” she says. Here, Nancy shares the strategies that have helped her manage diabetes, lose 120 pounds and regain her health:
Move past any guilt.
For decades, Nancy tried every diet out there, which inevitably led to feelings of deprivation and then loss of control. “I used to be like, Oh, well, I ate the pizza; I might as well have ice cream or something else for dessert,” she recalls. “I learned to say, Okay, you enjoyed it. Don’t feel guilty.” Nancy says it’s important to accept you will have setbacks—acknowledging that can make it easier to get back on a healthy track.
Learn your triggers.
Nancy learned that sugar is hidden in many everyday foods, even peanut butter and many frozen foods, and that sugar triggers her desire to eat even when she isn’t hungry. “I learned to read labels,” she says. “People don’t realize how much added sugar is in everyday foods. And I started learning to cook healthier.”
Personalize your plan.
When it comes to cooking, Nancy relies on the art of substitution. “I just kept looking at things and tailored my eating to my needs and desires,” she says. For inspiration, she recommends the Eat This, Not That! books and website as well as The Sugar Solution. “The other day I made a banana bread with cottage cheese,” Nancy says. “It’s high protein, and you don’t put sugar in it. It’s sweetened with pure maple syrup, which has a lower glycemic index. It’s an effective way for me to manage my blood sugar.”
Photo by Eliza Kommer
Photo by Eliza Kommer
“Focus on progress, not perfection!”
____________________
BRIAN BELOVITCH, 69
HUNTINGTON, NY
In 2007, after having a routine blood test, Brian Belovitch’s doctor told him he had pre-diabetes. “They wanted me to check my blood sugar, but I didn’t—I never took it seriously,” he recalls. “I knew what I was in for—my father had type 2 diabetes and was on insulin, and several of my siblings are pre-diabetic. I tried to stave it off by being careful with what I ate, but I never really succeeded.” Three years later, he was diagnosed with type 2 diabetes.
Despite being put on medication to lower his blood sugar levels, Brian still struggled to change his lifestyle, and his A1C (which measures a person’s average blood sugar levels over the previous three months) eventually increased to 7.5% (a normal A1C level is below 5.7%, 5.7% to 6.4% indicates pre-diabetes, and 6.5% and above indicates diabetes). In July 2024, his doctor prescribed a GLP-1 receptor agonist (GLP-1 RA).
Unfortunately, after starting the drug, Brian’s A1C remained at 7.5%. “I am such a junk food person,” he says. “I love candy bars, ice cream, cookies, chocolate and pastries. A lot of my eating habits were stress-related. If I got stressed out, I would eat sugar.”
Then, in November 2024, Brian’s doctor switched him to a different GLP-1 RA and the results have been remarkable—his A1C dropped to 6.2%, with his doctor expecting it to decrease further.
Inspired by his progress, Brian eliminated sugary treats and today walks about 5,000 steps daily. “My waist is two sizes smaller now,” he says proudly, adding that he’s lost more than 30 pounds. “Best of all, I feel so much better.” Here he shares the other tips he used to turn his health around…
Practice mindfulness.
Brian is a therapist and employs the same mindfulness techniques he teaches his patients to help keep his well-being in focus. “Be mindful of what you eat,” he advises. “If I want to have something sweet, I will have a piece of fruit or I have some yogurt with berries. Or if I’m out to dinner and everyone is ordering dessert, I have a spoonful or a taste of whatever they are having and try to focus on savoring it. It’s really about not denying yourself but being aware of what you’re eating—including how it makes you feel afterward.”
Treat yourself with compassion.
Brian emphasizes treating yourself with kindness through the diabetes journey. “It’s progress, not perfection,” he says. “We all indulge sometimes, but you can’t let that derail you.”
Follow medication guidelines.
“I was very patient and compliant with taking my new medication as prescribed,” Brian says. “Setting a regular schedule and using reminders like alerts on your phone can make it easier. It’s also important to ask your healthcare provider when you’ll start seeing results—that way if the medication maybe takes some time to kick in, you won’t feel discouraged.”
Photo by Brittany Breen Photography
Photo by Brittany Breen Photography
“Reach out for help.”
____________________
ROGER HARE, 50
CINNAMINSON TOWNSHIP, NJ
About seven years ago, Roger Hare felt constantly thirsty and seemed like he was constantly needing to urinate. He also developed poor vision, and his energy levels plummeted. For many years, his doctor had told him he had pre-diabetes, but that didn’t stop the accountant from eating the chocolate cake he loved and adding sugary creamer to his coffee.
Then in June 2019, after a visit to his family doctor, blood tests showed his A1C had skyrocketed to 12.7%, and he was diagnosed with type 2 diabetes. Roger felt overwhelmed. “I started reading nutrition labels, and I almost had a nervous breakdown in the middle of the grocery store,” he recalls. “I realized all the food that I love to eat—the processed foods, the pasta, the chocolate cake—I couldn’t have any of it.”
Then Roger spoke to a cousin whose husband had diabetes and received some advice that helped him focus and take positive action. “She said, ‘It’s not about never eating cake again. You need to limit your carbohydrates to what’s right for you,’ ” he recalls. “So I downloaded an app and started counting carbs and tracking everything.”
As a result of swapping processed foods and white rice for colorful vegetables, exercising in a gym and walking, as well as taking diabetes medication, his A1C eventually dropped from 12.7% to 6.0%, and he intentionally lost 40 pounds within five months. Here are the other methods Roger used to get his blood sugar under control…
Find the right care team for you.
“When I was first diagnosed by my family doctor, he said to me, ‘You need to diet and exercise,’ ” Roger recalls. Wanting some more guidance, Roger sought to find a new healthcare team that would provide him with more insight on the right treatment for him. He soon connected with an endocrinologist and a new primary care physician, both knowledgeable about type 2 diabetes, who helped him further. He also turned to the American Diabetes Association (ADA) for educational resources.
Be your own advocate.
Roger wears a continuous glucose monitor on his arm to check his blood sugar, and last year he noticed that his readings when he first woke up were elevated. He shared the news with his physician, who prescribed a weekly injectable medication. “My A1C dropped from a high of 7.6% at the end of May to 6.0% in mid-November after that,” says Roger, noting his A1C is now the lowest it’s been for at least 15 years.
Get involved.
“I’m big about being held accountable,” says Roger, who has done fundraising for the ADA and traveled to Washington, DC, to advocate for increased funding for diabetes research. “One of the reasons why I am involved with the ADA is I can go there to have conversations with people about my diabetes. Not only do I learn things, but I can also share with others what I’ve learned and it makes me feel good knowing I can help others. I encourage people who are newly diagnosed to take baby steps and to reach out for help.”
Q&A
Experts answer your questions about diabetes

HELP, I’M FEELING OVERWHELMED!
Q: I just got diagnosed with type 2 diabetes, and from testing blood sugar to calculating meals, it’s too much to handle! How do I make it less stressful?
A: Give yourself time to get used to your new routine—once you learn the appropriate amount for certain meals, it will become ingrained. Try carbohydrate consistency: Eat the same amount of carbs with each meal so you can keep the insulin constant as per your carbohydrate ratio. If you’re feeling overwhelmed, talk to your certified diabetes educator.
—Alethea Shepardson, FNP, CDE,
diabetes management specialist at Montefiore Health System, NY
FIXES FOR NEEDLEPHOBIA?
Q: I have type 2 diabetes, and I hate needles. Are there any alternatives to using injectables?
A: Yes, there are many new needle-free, non-insulin oral medications, as well as injectable options you may need to take less often. Also, many injectable types now come in pre-filled pen form—the needle itself is tiny so you’ll barely feel it. Ask if you’re eligible for a continuous glucose monitoring sensor, a wearable device with a tiny sensor inserted right under your skin that tracks your blood sugar levels 24/7.
—Rachel Pessah-Pollack, MD, FACE,
Clinical Professor, Division of Endocrinology, Diabetes & Metabolism,
NYU School of Medicine, NYU Langone Health
Stay on your toes with these foot-friendly moves!

If you have diabetes-related neuropathy, your feet may bear the brunt of it. The nerve condition can cause burning pain and loss of feeling, make you prone to foot sores and impair your ability to walk properly. Luckily, physical therapist Frank Musumeci, founder of Prescription Exercise, a preventive orthopedic fitness clinic in Miami, says giving your feet some TLC can help keep them in top shape.
KEEP YOUR FEET FLEXIBLE
If you have to wear tight or pointy shoes—say, for a dressy occasion—try this stretch before and after the event:
Sit down, place your feet side by side and loop a thick elastic band around your big toes. Slowly pull your big toes apart to gently stretch the ligaments and joints. Hold for 10 seconds; repeat five times.
Don’t do this: Wear heels over two inches. Anything higher puts too much pressure on your forefoot, especially the big toes.
LOOSEN YOUR ANKLES
To prevent pain, the bones between your ankle and shin need to glide easily over each other. This move can help:
Sit on a chair, raise one foot slightly off the floor and “write” each letter of the alphabet with your big toe. Repeat with the other foot. If your ankle doesn’t have full range of motion, physical therapy can help restore movement.
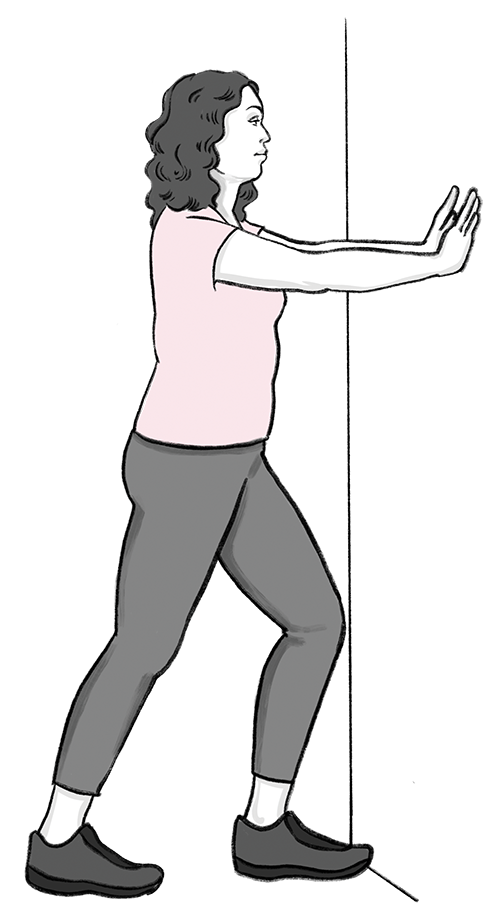
STRETCH YOUR CALVES
Flexible calves provide a stable base, helping you to walk more efficiently and preventing falls. Stretch after a shower, when your muscles are warm and pliable. Two exercises to try:
Wall stretch:
Lean against a wall, hands flat, with your left foot forward and right foot back. Keep both heels on the floor and press your hips forward, feeling the pull in your right calf and Achilles tendon. Hold for 30 seconds, then switch sides. Repeat three or four times.
Towel stretch:
Sit on the floor with both legs out in front of you. Loop a towel around the ball of one foot and pull the towel toward you, keeping your leg straight. Hold for 30 seconds, then switch sides. Repeat three or four times.
Cushion your landings
For everyday wear, opt for shoes with a rubber sole and a wide toe box. The shoe should also bend at the ball of your foot where you push off, not in the middle.
Easy footwear test:
If you can fold the shoe in half, skip it.
Tip! Always check your feet daily for ulcers or cuts and make sure to avoid walking barefoot.
Illustrations by Juhee Kim
Sneaky reasons your blood sugar is...
High
1. You skipped breakfast.
Bolting out the door without eating in the morning can mean higher blood sugar the rest of the day. Studies suggest that when you skip breakfast, you’re likely to experience hyperglycemia (high blood sugar) after lunch due to decreased insulin and GLP-1 secretions. This impaired glucose regulation may extend to later meals as well, contributing to higher blood sugar levels.
Try this! Prep blood sugar-friendly breakfast options on the weekend and freeze for time-crunched weekday mornings.
2. You eat a high-fat diet.
Regular high-fat meals can cause blood sugar to rise in two ways: First, high-fat meals result in more free fatty acids in your blood, causing insulin resistance and difficulty moving blood sugar into cells. Second, fat slows the release of blood sugar, so insulin can be done working before blood sugar even builds in the blood.
Try this! Stay away from fast food because fried fare has a high amount of saturated fats. Instead, try packing a lunch or meal prepping whenever you can so you have full control of the nutrients in your meal.
3. You haven’t slept enough.
Feeling tired can cause you to reach for food—and in particular comfort food—more often than you would if you were rested, which may lead to high blood sugar levels. Plus, not getting enough rest can trigger a rise in blood sugar-raising stress hormones.
Try this! If you often fall short on the amount of sleep you need—and you don’t see a solution to that right now—ask your doctor if timing your insulin or oral medication differently could help.
4. You got sick.
Coming down with the flu, a cold or other illness triggers the release of stress hormones that lower your body’s ability to use insulin, so blood sugar rises.
Try this! Monitor your blood sugar more often while you’re sick and drink water to stay hydrated and flush blood sugar through your system. Check with your diabetes care team to see if you need to temporarily adjust your meds.
Low
1. You used too much insulin/medication.
Taking more insulin than you need can cause your blood sugar level to drop too low, which can cause hypoglycemia. Signs include shakiness, anxiety, sweating, chills, clamminess, nausea, confusion and rapid heartbeat.
Try this! Eat a source of quickly absorbed sugar—aim for 15–20 g of carbs, such as 5–6 oz of orange juice, 6 Hershey Kisses or 15 Skittles. (If you prefer glucose tablets, check the nutrition info on the label, as the amount of carbs varies by brand.) Then work with your diabetes care team to find the right dosage and schedule to fit your diet and activity habits.
2. You took a hike—but didn’t plan for it.
Your muscles use glucose (sugar) in your blood during exercise and activities like yard work or housecleaning, causing blood sugar levels to fall. If you don’t eat enough to cover your activity, your levels can drop too low.
Try this! Set a time on your watch to remind you to stop and have a snack, and keep portable snacks handy when away from home.
Be on guard for: Hypoglycemia unawareness, which is when you don’t feel any symptoms (such as shakiness, sweating and nausea) when your blood sugar drops below 70 mg/dL. If this happens, ask your care team if changing your blood sugar targets could help you avoid future episodes or if you might be a candidate for a continuous glucose monitor.
3. You drank (alcohol) more than you ate at a party.
Alcohol can cause your body to release too much insulin, causing severe low blood sugar. Drinking alcohol on an empty stomach can heighten this impact, since your liver is working on removing the alcohol from your blood instead of managing blood sugar levels.
Try this! Test your blood sugar before and up to 24 hours after drinking and have a snack if you find it’s low. It’s also important to limit your alcohol intake to one drink a day for women and two drinks a day for men.

Sweets?
Yes, please!

Think desserts are off-limits? Not true! Having diabetes doesn’t mean you have to give up Aunt Betty’s pecan pie or Grandma Ethel’s from-scratch peach cobbler. Read on! —by Constance Brown-Riggs, MSEd, RDN, CDCES, CDN
You can have your cake—and keep your blood sugar within range, too. In fact, the American Diabetes Association says that desserts can be part of a healthy diet. Here are some strategies for doing just that:
Budget for it.
If you want to have that brownie, find out how many carbs it has (for a packaged food, check the nutrition label; if you’re dining out, try the restaurant’s website; and for homemade eats, enter the ingredients into the analyzer at happyforks.com/analyzer), and budget for it throughout the day.
Check your levels.
A chocolate chip cookie might cause your blood sugar to skyrocket while bread pudding doesn’t. The only way to know for sure? Check your blood sugar! Test two hours before and after eating a sweet to see how it affects you. It can help guide your choices and your portion sizes, too.
Fill your dessert plate this way.
Try half a slice of cake and fill the rest of your plate with nuts or berries to balance it with fiber and nutrient-dense foods.
Make it yourself.
That way, you can control the ingredients. For example, you can cut sugar by using substitutes like stevia, sucralose or monk fruit, or use berries, apples or other fruit for natural sweetness. To cut back on saturated fat, you can replace the butter or oil with Greek yogurt. And instead of white flour, use whole wheat flour.
Time it right.
Forget the saying “Life is short, eat dessert first.” Turns out saving treats for the end of a meal is a smart move for people with diabetes. One study shows that eating proteins and fats before your carbs—like having steak before dessert—can help prevent blood sugar spikes after meals. The reason: Proteins and fats slow down digestion, help your body release insulin at the right time and keep insulin in your system longer. Another way to slow digestion—and feel full longer—is to include high-fiber foods like whole grains, legumes, fruits and vegetables in your main meal.
Your new go-to dessert!
This cobbler gets most of its sweetness from fruit, and odds are you already have most of the ingredients in your pantry. If you keep frozen peaches and berries on hand, you’ll always be able to whip it up when the mood strikes.
One serving equals one serving of fruit!
Peach and Blueberry Cobbler
Makes 8 servings
For filling:
- 2 cups peaches, cut in chunks (frozen or fresh)
- 1 cup blueberries (frozen or fresh)
- 2 Tbsp brown sugar
- 1/2 tsp cinnamon
- 1/4 tsp ground nutmeg
- 2 Tbsp cornstarch
- 1 Tbsp canola oil
For topping:
- 1 cup whole-wheat flour
- 1/4 cup white sugar
- 1/4 cup brown sugar
- 1 tsp baking powder
- 1/2 tsp salt
- 6 Tbsp butter, unsalted
- 1/4 cup boiling water
Preheat oven to 425°F.
Combine peaches, blueberries, brown sugar, cinnamon, nutmeg and cornstarch in a bowl. Make sure fruit is well-coated.
Using the oil, grease a 1½-quart casserole dish. Pour fruit mixture into dish.
Bake in oven for 10 minutes; remove and raise oven temperature to 435°F.
While fruit is baking, make topping. Combine flour, sugars, baking powder and salt in a bowl.
Blend in butter with your fingers or with a pastry blender until mixture is coarse, then stir in water.
When filling is done baking, drop spoonfuls of the topping onto the mixture and bake at 435°F for about 30 minutes.
Nutrition facts: Calories 232, Fat 9 g (Saturated Fat 5 g), Cholesterol 25 mg, Sodium 200 mg, Carbohydrate 35 g, Fiber 3 g, Sugar 20 g, Protein 3 g
Source: Med-South Cookbook ©2020 UNC-CH Center for Health Promotion and Disease Prevention
6 ways to keep your vision clear!

If you have diabetes, you know that high blood sugar can affect your entire body, including your eyes. In fact, diabetes is the leading cause of blindness in adults, according to the Centers for Disease Control and Prevention. In addition to aiming for your target A1C, minimizing blood sugar spikes and dips, and getting regular exams, try these strategies:
1. Stub out cigarettes.
Not only does smoking make it more difficult to control blood sugar, research shows that smokers have double the risk of developing cataracts than nonsmokers, and heavy smokers (15 cigarettes/day or more) have three times the risk! If you smoke and are having trouble quitting, ask your doctor about smoking cessation treatments and consider joining a support group to learn techniques that can help kill the cravings.
2. Slash stress.
Anxious jitters do more than just frazzle your nerves; stress can also raise blood sugar and blood pressure, both of which may damage blood vessels in the eye. In fact, a study published in the American Journal of Ophthalmology found that chronic stress is a risk factor for developing glaucoma. So whenever you feel overwhelmed, turn to your favorite soothing technique.
3. Sport shades.
People with diabetes are at a greater risk of cataracts because consistently high blood sugar causes blood vessels in the eyes to swell and accelerates the thickening of your eyes’ lens, according to the American Diabetes Association. Since direct exposure to UV light is another contributing factor, be sure to wear sunglasses every time you go outside, rain or shine. Choose a pair that blocks 100% UVA and UVB rays.
4. Deflate high blood pressure.
Untreated high blood sugar can lead to diabetic retinopathy (DR), in which blood vessels in the retina get damaged. Fortunately, studies have found that getting blood sugar levels to a normal level reduces the risk of developing DR. Your healthcare provider may recommend adding a medication to reduce blood pressure and making lifestyle changes such as increasing activity and eating a healthy diet.
5. Ramp up your heart rate.
Aerobic activities like walking, biking and dancing can help keep eyes healthy by reducing pressure on the nerves in the eye. In addition, exercise can lower high blood sugar levels, cholesterol and blood pressure, all of which can contribute to eye disease. Research published in Microvascular Research found that those who get regular moderate-intensity exercise can keep DR from progressing.
6. Get hooked on fatty fish.
Fish that is rich in omega-3 fatty acids, such as salmon, tuna, mackerel, halibut and sardines, may protect against DR by preventing inflammation and abnormal blood vessel growth in the eyes. In fact, a study published in Experimental Eye Research suggests that consuming 1,000 mg per day of omega-3s (that’s four servings a week of fatty fish) can lower the risk of DR.
The best protection?
Regular eye exams!
Often, symptoms don’t appear until a disease has progressed. Having regular eye exams is the best way to catch eye disease early.
Quiz
Paid Advertiser
Special thanks to our medical reviewer:
Lubaina S. Presswala, DO, FACOI, FACE, Endocrinologist, Assistant Attending Physician, Memorial Sloan Kettering Cancer Center, New York.
Content reviewed by:
AACE is not responsible for statements and opinions of authors or the claims made by advertisers. The appearance of advertising does not imply endorsement of or guarantee the claims of the advertisers.
Lindsay Bosslett, Vice President, Editor-In-Chief; Joana Mangune, Editorial Manager; Amanda Prost, Editor; Sara Rotondi, Associate Editor; Debra Koch, Senior Copy Editor; Maria Lissandrello, Editor Emeritus; Erica Kerber, Vice President, Creative Director; Suzanne Augustyn, Senior Art Director; Kimberly H. Vivas, Senior Vice President, Production and Project Management; Rachel Pres, Senior Director, Digital Production
Dawn Vezirian, Senior Vice President, Financial Planning and Analysis; Tricia Tuozzo, Senior Manager, Client Solutions, Key Accounts; Augie Caruso, Executive Vice President, Sales and Key Accounts; Keith Sedlak, Executive Vice President, Chief Commercial Officer; Neil Glass, Chief Financial Officer; David M. Paragamian, Chief Executive Officer
Health Monitor Network is the nation’s leading multimedia patient-education company, with websites and publications such as Health Monitor®.
For more information: Health Monitor Network, 11 Philips Parkway, Montvale, NJ 07645; 201-391-1911; healthmonitornetwork.com ©2025 Data Centrum Communications, Inc. Questions? Contact us at customerservice@healthmonitor.com
This publication is not intended to provide advice on personal matters, or to substitute for consultation with a physician.
LUJ25-DG-TD-1EZOGM
Health Monitor Medical Advisory Board
Michael J. Blaha, MD, Director, Clinical Research, Ciccarone Center for the Prevention of Cardiovascular Disease; Professor of Medicine; Johns Hopkins
Leslie S. Eldeiry, MD, FACE, Clinical Assistant Professor, Part-time, Department of Medicine, Harvard Medical School; Department of Endocrinology, Harvard Vanguard Medical Associates/Atrius Health, Boston, MA; Chair, Diversity, Equity and Inclusion Committee, and Board Member, American Association of Clinical Endocrinology
Cheri Frey, MD, Assistant Professor of Dermatology, Howard University; Chair, Dermatology Section, National Medical Association
Marc B. Garnick, MD, Gorman Brothers Professor of Medicine, Harvard Medical School; Director, Cancer Network Development, Beth Israel Deaconess Medical Center; Editor-in-chief, Harvard Medical School’s Annual Report on Prostate Diseases
Angela Golden, DNP, FAAN, Family Nurse Practitioner, former President of the American Association of Nurse Practitioners (AANP)
Mark W. Green, MD, FAAN, Emeritus Director, the Center for Headache and Pain Medicine; Professor of Neurology, Anesthesiology, and Rehabilitation, Icahn School of Medicine at Mount Sinai
Mark G. Lebwohl, MD, Dean for Clinical Therapeutics, Professor and Chairman Emeritus, Kimberly and Eric J. Waldman Department of Dermatology, Icahn School of Medicine at Mount Sinai, New York
Maryam Lustberg, MD, Associate Professor of Internal Medicine (Medical Oncology); Director, Center for Breast Cancer; Chief, Breast Medical Oncology; Yale School of Medicine
William A. McCann, MD, MBA, Chief Medical Officer; Allergy Partners, Asheville, NC
Mary Jane Minkin, MD, FACOG, Clinical Professor, Department of Obstetrics, Gynecology, and Reproductive Sciences, Yale University School of Medicine
Rachel Pessah-Pollack, MD, FACE, Clinical Professor, Division of Endocrinology, Diabetes & Metabolism, NYU School of Medicine, NYU Langone Health
Stacy K. Silvers, MD, Chief Medical Officer, Aspire Allergy & Sinus, Austin, TX
Julius M. Wilder, MD, PhD, Associate Professor of Medicine; Vice Chair, Equity, Diversity, and Inclusion; Duke Department of Medicine